Sands comments on progress in implementing the recommendations of the 2013 Health and Social Care Committee’s Stillbirth Inquiry - December 2014
In Wales approximately 1 in 220 babies delivered after 24 weeks gestation are stillborn each year.
153 babies were stillborn in 2013, meaning three babies are stillborn every week in Wales.
Many stillborn babies are born perfectly formed; many are born at or near the end of pregnancy when their death might have been avoided with timely delivery.
The stillbirth rate in Wales remains largely unchanged, unlike neonatal death rates which have fallen significantly in the last decade.
Every baby’s death leaves a family devastated, with the impact enduring for years if not lifetimes. Wider family, friends and health professionals too are affected, multiplying the impact.
“I had thought that terms like ‘your arms aching to hold him’ belonged in trashy romance novels. But they are true. Your arms do ache. Your chest does feel as if a huge stone has settled on it. Your heart does break into a million pieces. It’s the loneliest feeling in the world.” Bereaved mum.
Stillbirth rates in Wales and other UK countries, 2008 – 2013
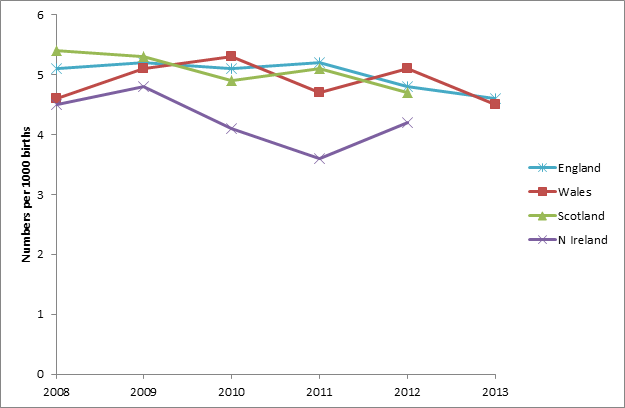
*Source Office for National Statistics. Death Registrations Summary Tables, England and Wales, 2013
Background
Sands was among those who contributed written and oral evidence to the Welsh Government’s Health and Social Care Committee’s inquiry into stillbirth in June 2012, which reported in February 2013.
Sands has closely supported the work of the Welsh Initiative for Stillbirth Reduction (WISR), the national stillbirth group set up in April 2012, which was carrying out a range of work-streams, as detailed in the WISR final report of March 2014. Since March the group has been suspended, pending the re-organisation of maternity services and staff recruitment.
The suspension of WISR has led to a hiatus in the co-ordinated approach to stillbirth reduction work in Wales. Because of that we are not able to report in detail on progress at a national level since March this year, but just on the initiatives we are directly working on.
Sands contributes to the Wales Perinatal Pathology sub-group, looking at the availability of perinatal pathology services and improving parents’ experience of the post-mortem process.
Sands is driving, or closely involved with, a number of significant UK-wide stillbirth reduction initiatives, which have included Welsh input, and are described in our response.
Our response includes personal reports from parents in Wales. Sands has seven support groups covering regions across Wales, co-ordinated through the Sands Welsh Network. We asked parents, via our Facebook and the Welsh Network, to contribute their experiences and views of care since the stillbirth inquiry made its recommendations.
One mother said, “It has been tough. I am glad to hear that parts of my submission will be used. I just hope that through sharing personal experiences improvements will be made, resulting in a reduction in often unnecessary stillbirths.”
Recommendation 1
Public awareness of stillbirth and its risk factors is essential to reducing stillbirth rates in Wales. We recommend that the Welsh Government take an active lead – via the recently established National Stillbirth Working Group – in developing key public health messages as a matter of priority. This will raise the awareness of expectant parents and those planning to start a family of the risks of stillbirth and allow them to make more informed choices about their health and pregnancy.
Recommendation 2
We recommend that the Welsh Government work with professional bodies and health boards in Wales to ensure that all expectant parents receive adequate information from clinicians and midwives about stillbirth and its associated risks. Discussion of stillbirth should form a routine part of the conversation held between health professionals and expectant parents during the course of a pregnancy.
Parents feedback:
“I would say that the issue of Stillbirths is still far too taboo a subject. While new expectant mothers do not want to be scared off with horror stories, I still think more education on reduced / increased movements should be promoted. My own midwife was excellent, but I think she, along with the other midwives, are at times over stretched and do not want mums to be coming in to be checked all the while.”
“In July 2013 we experienced the stillbirth of our Daughter at almost 30 weeks gestation. Having had a maternity-led and an “easy” pregnancy this was a total shock. Due to lack of movements all day, that evening I contacted the Labour ward to be told to lie on my side for 2 hours to monitor movement, despite me stating that I had felt no movement that day. We insisted on a scan that evening. An ultrasound confirmed that she had passed away in-utero. During my pregnancy I had received very little information from my midwife regarding monitoring movement - I was given a brief leaflet at 24 weeks and told to be concerned if the baby moved too little or too much, with no description of what that meant. More information on how to correctly monitor movements is required for all mums to be. “
The Welsh Government’s progress report includes an up-date on the work Sands has been leading, in collaboration with DH England, to develop public health messages on stillbirth risk. The Public Health Task and Finish Group we brought together to guide this work includes stakeholders from the relevant professional bodies, parent groups and devolved countries, including Wales: our aim has been for UK-wide agreement on the key ‘safer-pregnancy’ messages for pregnant women.
Further to the up-date, we have now drafted, with the DH England, a consensus document with the core messages, which stakeholders are invited to sign up to. We would welcome Welsh Government support for this document.
Alongside the core messages, the group has agreed a narrative for the messages, which can be used to guide the wording of information resources. These include agreed wording for guidance on fetal movement monitoring.
DH England now aims to convene a group to agree a strategy for effective dissemination of the agreed key messages. We would welcome continued Welsh input in this process. Clearly the development of information platforms, be they leaflets or a web solution, will require funding and we would welcome support from Welsh Government for this next stage.
In late 2013 Sands commented in detail on the Bump, Baby and Beyond pregnancy booklet, using our feedback at that time from the Public Health T&F group as well as the focus groups of parents and midwives (which included a focus group in Cardiff). We would suggest Welsh pregnancy information is reviewed again in light of the finalised core messages and narrative around stillbirth risk.
Recommendation 3
We recommend that the Welsh Government work with professional and regulatory bodies, and relevant academic institutions, to ensure that stillbirth, its associated risk factors and interventions, and bereavement training are more prominently featured in Welsh
midwifery and obstetric training curricula. The Welsh Government should work with health boards to monitor and regularly review the training needs and competence of health professionals in relation to stillbirth.
Parents feedback – care in pregnancy:
“We believe the following issues contributed to our baby being stillborn:
Failure to interpret test results (specifically CTG and fundus height measurements over a 6 weeks period) leading to non-intervention of a pregnancy.
Failure to read maternity notes and pull the bigger picture together. There were a number of indicators that when viewed together would have strongly indicated that there was a problem and further tests should have been implemented.
Assumption that a ‘low risk’ pregnancy does not warrant closer inspection, despite warning signs. Low risk=no clinical rigour is not acceptable!”
“Towards the end of the pregnancy I was in for daily fetal heart monitoring, and this was at the request of fetal med. At the weekend this was in the emergency pregnancy unit. Outside the door I could hear a midwife moaning that I was in again, and at a weekend, and she saying that she couldn’t see why. Later in that appointment no heartbeat could be found in our son.”
Sands comment - Stillbirth risk:
In 2012-13 WISR led a series of learning days for maternity professionals from Health Boards across Wales at which there were presentations on a range of stillbirth risks and interventions and productive discussions with action-plans to take away. Topics included: improving the detection and management of poor fetal growth; improving protocols for responding to a mum’s report of reduced fetal movements; and how to encourage up-take of post-mortems.
We cannot comment on progress of training for professionals with regards stillbirth risk since March 2014. For example, all Health Boards had undertaken to identify funding to implement the GAP (Growth Assessment Programme) training programme to improve detection of growth restricted babies - we do not know if this is now in place across Wales.
Parents have reported to us that pressures on staff and understaffing are leading to rushed and sometimes poor care. Staffing levels are an issue which needs to be looked at alongside improving staff knowledge and awareness around stillbirth risk assessment.
Parents feedback - bereavement care:
“Sadly I can’t say anything other than the [bereavement] care was horrific. It felt like there wasn’t a care pathway which I fell into so I just fell between the cracks. I got through, just about, by being insistent.”
“The level of care I received following my discharge from hospital was poor. I received 1 visit from the midwife and 1 from the Health Visitor. My C-section scar subsequently became infected, which resulted in another hospital stay, which was distressing as the room I was located in was next to the labour ward and me and my husband could hear baby heart monitors and babies. I did request bereavement counselling, with a specialist in child loss, but my local Health Board were unable to assist me. I feel that following my hospital discharge the care and support I have received was not sufficient.”
“Generally good but it is disappointing that there is no bereavement midwife available. We have also had to organise our own counselling.”
“When my little boy was born in May 2014 …I was left in the bereavement room in which I could hear mothers going into labour and babies crying all night, which was heart wrenching. I was discharged a few days later and since then I have not received any care, follow ups..nothing!”
“I was in hospital, in labour, for 4 days and I found it very difficult that there was no consultant available at the weekend and even during the week that there was a different consultant on each day each giving differing opinions and advice, there was no continuity of care at all. After my daughter died I stayed in hospital one more day and the midwives were as helpful as they could be….I found that there was a complete lack of after care once I was discharged, I didn't speak to another healthcare provider after that. This is by far the worst experience of my life, and would have always been, but the casual attitude of the staff made it so much more stressful and painful than it should have had to.”
“The postnatal care lets women down. We need more midwives in Wales!! Our postnatal ward is run by 2 or 3 midwives looking after 40 women & their babies.”
“During the birth I was supervised by a midwife and a student, the final part was quite swift and the student was unattended and clearly upset herself, and was in the corridor shouting for someone to come, while the food lady was knocking with her trolley.
Immediately after giving birth the midwife said she wasn’t sure how to complete the paperwork – and could we come back tomorrow. We were then left alone with our son to say good bye. Whilst this was fine, and we didn’t feel too hurried it felt odd to be leaving hospital at midnight after giving birth with no health advice. The next day I was told that the community midwife would call, again no health info or SANDS info was given, other than an incomplete SANDS memory box. Over the next few days the midwife didn’t call. Then out of the blue she did… she was clearly very uncomfortable at the situation. She went so far as to say she wasn’t sure what to say as she hadn’t been in the situation herself, and not to be surprised if others found it awkward.”
“I didn’t receive a call about a 6 week postnatal check-up, so I called the GP surgery and explained to the secretary. A GP called back, and ask why there was a need as there was no baby to check, but I could call in to talk about contraception.“
Sands comment - bereavement care:
Parents responded in greatest detail with regards the care they had received after their baby died. Sadly almost all reports we received for this submission were of poor care. We do know through our support groups that many health care professionals in Wales deliver sensitive and caring support to parents after a baby dies, and we would emphasise that the feedback above does not reflect this positive side.
However it is clear that there are still too many unacceptable instances when poor care is adding further distress to the aguish parents already experience when their baby dies. Staff are too rushed to offer good care or ill-prepared in understanding what good care means; communication with parents is inadequate; or bereavement facilities are lacking. We would welcome a more detailed review of bereavement services in Wales - including care during delivery, post-natal care and care after parents leave the hospital and return to community services – to look at what needs to be done to ensure a high quality, complete pathway of care for all parents at this already desperately painful time.
For many years Sands has offered training in bereavement care to compliment our Guidelines for Professionals book. In 2013 we carried out a comprehensive review of our training programme. A revised workshop format was piloted, including a pilot day for midwives at Nevil Hall Hospital, Abergavenny, in February 2014. Health professionals’ feedback was incorporated into the final version of our new skills-based Bereavement Care Training programme. We have subsequently been awarded professional accreditation from the Royal College of Midwives.
In June 2014 Sands ran a successful half-day course for student midwives at Cardiff University. Evaluations were strongly positive indicating those who attended felt more confident about communicating sensitively and effectively with bereaved parents as a result of the training.
One participant said, “The insight into experiences of real stories and the parts on communication skills were very useful as was the variety of the session... It was very useful and will benefit my practice. “
We plan to promote and deliver our Bereavement Care Training programme for midwives, student midwives and multi-disciplinary groups throughout Wales. We would welcome support in encouraging Health Boards to take up this training.
Recommendation 4
We recommend that the Welsh Government scope the viability of establishing a maternity network to drive the standardisation of care across Wales. We believe that at least a virtual clinical network should be established within the next 12 months.
Sands cannot comment on progress with regards the maternity networks. However we are concerned that the absence of a national forum to focus on stillbirth has led to a loss of momentum on stillbirth work.
We will welcome an early resumption of a WISR-style national stillbirth group within the new maternity networks, to ensure a national focus continues on the urgent issues of stillbirth reduction and bereavement care.
Recommendation 5
We recommend that the Welsh Government undertake a review of the number of women in Wales who deliver more than thirteen days after their due date. The outcome of those pregnancies and the factors that led to the decision not to induce within the recommended guideline time should be considered in every case. Further consideration ought to be given to whether women with other high risk factors such as advanced maternal age, smoking or weight should be induced closer to their due date.
We cannot comment on progress with regards this recommendation.
Recommendation 6
We recommend that the Welsh Government investigate and report on evidence presented to the Committee that having to seek specialist foetal medicine consultations outside Wales now exceeds the cost of providing the service within Wales. The Welsh Government should also explore the proposal that specialist foetal medicine services should be commissioned at the tertiary rather than secondary level.
Sands cannot comment in detail on this recommendation.
However feedback from parents indicates that specialist fetal medicine services where they are available in Wales are “overworked and under-staffed”.
Recommendation 7
We recommend that a national minimum standard for reviewing perinatal deaths should be developed and rolled out across Wales. We also recommend that a wider, more imaginative approach to Welsh Government funding for medical research and investigation is adopted, and that the Welsh Government seek detailed costings for a national perinatal audit for Wales from the All Wales Perinatal Survey. We believe that the initial investment in this audit could yield significant benefits in the future detection and prevention of stillbirth.
Parents feedback:
“Our previous pregnancy ended in a prem baby who was tiny for dates. No investigation was undertaken. After next pregnancy (which ended in stillbirth) the post-mortem identified that I have a condition which leads to poor placental performance, and which can be improved by certain drugs early in pregnancy. In some NHS hospitals it is policy to investigate placentas of babies who are small/prem but survive – but not in ours. I asked our consultant if an investigation of the 1st placenta had happened could the outcome of the second pregnancy could have been different – she went quiet and said that now there was no way of knowing. I wonder if investigations had been carried out after the 1st pregnancy there might have been a different outcome for our stillborn son.”
As described in the Welsh Government’s progress report, Sands has been leading a multidisciplinary Task & Finish Group looking at perinatal mortality review. The UK-wide group includes Welsh input. It is accepted that the quality of the review process for investigating perinatal deaths varies greatly and urgently needs improvement and standardisation to ensure lessons are learnt and changes to care are implemented.
The group has completed work on a core data set for review, including a taxonomy, grading of care and the generation of an action plan for improvements to care. We have set out principles to underpin perinatal review.
This work has been handed to DH England to take to the next stage, which is to turn the data set into a usable review tool via a web platform. We believe a web-based system is most practical: this approach was successfully piloted by the Perinatal Institute’s SCOR system in 2012, against which this collaboratively-developed tool was benchmarked.
The DH is undertaking a cost /benefit analysis of developing a standardised review tool which Sands has contributed to.
In October 2014 a meeting was held with all four UK governments to discuss working collaboratively to develop a review tool for UK-wide use. There was support for the work and an agreement to draw up a specification for the IT work to develop and run a web-based tool, in order to assess the potential costs and data governance issues.
We would welcome continued Welsh Government support in developing this work, and ultimately in contributing to funding the development of the review tool.
Sands is a partner in MBRRACE-UK, the national Clinical Outcome Review Programme, which has taken on the collection of perinatal mortality data across the UK, including Wales, from 2013. The first report on the 2013 perinatal data will be published in June 2015.
Recommendation 8
We recommend that the Welsh Government publish a detailed plan of how it proposes to tackle the problem caused by the low rate of post-mortem for stillborn babies. The plan should include:
- details of how training will be delivered to health professionals in order that they are better equipped to raise this very difficult issue with grieving parents;
- details of what improved information will be developed for parents so that they are able to make more informed decisions; and
- an assessment of the actions needed to improve the provision of perinatal pathology.
Parents feedback on post-mortem:
“After we went home I heard nothing more from the bereavement midwife. I had to contact her after 6-7 weeks to ask about PM results. She said she would chase up. I heard nothing after a week so I found the consultant details and made contact myself. I had the PM appointment 10 weeks after he died. I found this far too long. It was an agonising wait to merely to be told 'no known cause'.”
“During my time with our daughter we felt bombarded by the Bereavement midwife (who was not the midwife taking care of us) to make a decision regarding the consent for a post mortem. She left a leaflet for us to read regarding the process and she acted as though this was a normal situation - with little sensitivity or compassion. The Bereavement Midwife wanted a decision on the same day we had said goodbye to our daughter – it was too much. We decided the following day to a full post-mortem.”
“I found it particularly difficult that we were given a time frame of 6-8 weeks for PM results when in fact the PM took four months to be ready; it then took a further three months, so a total of seven, for us to see our consultant and get the results of the PM report. I had to call the hospital at each juncture to push things along. I'm sure we still wouldn't have heard anything had I not.”
“The post mortem was undertaken within days of our baby being born in October; however our appointment to go through it was not until the end of January. We were told that this was due to the time taken to write it up.“
“We were happy with our PM experiences. There is a long wait for the results, but we appreciate this is necessary to ensure completeness and rigour. “
“It was 9 weeks until we met the consultant for the post-mortem report – there should be a maximum waiting time for results and feedback appointments with consultants should be treated urgently. It was due to constant phone calls and pleading that we had feedback within this timescale.”
Sands contributes to the Wales Perinatal Pathology sub-group, which has looked at improving post-mortem up-take and at capacity issues for specialist perinatal post-mortem services. This group reported separately in March 2014, with full recommendations. We have no up-date since March on the progress of implementing those recommendations, including the urgent capacity issues also raised by Sands in our original inquiry submission.
In 2013, in collaboration with key stakeholders and the Human Tissue Authority, and after extensive consultation with parents, Sands completed a Perinatal Post Mortem Consent Takers Package, including a standardised consent form, and an information booklet for parents. While it was decided not to make use of the consent package in Wales, Sands helped to revise the Wales parent information book in line with the Sands booklet.
Recently Sands has looked at the issue of delays in reporting back to parents on the outcomes of the post-mortem. National recommendations are that the report should be returned within six weeks; however our experience suggests 12 weeks plus is normal. Delays contribute to parents’ reluctance to consent to post-mortem. Some of the issues, besides service capacity, identified as contributing to delays are:
- If the consent taker is poorly trained then this affects how well the consent form is filled in. We know of cases where consent forms have had to be re-done because they were badly filled out.
- Some babies’ bodies are sent to the pathologist in batches, leading to delays for some parents. We recommend hospitals review their processes for transferring babies to avoid this.
- The way reports are returned to hospital can introduce delays e.g. by mail rather than email. Furthermore the way follow-up appointments are booked can lead to further delays adding 2-3 weeks to the period from when the report reaches the hospital to when it is shared with parents.
All of this is extremely distressing to parents. We would like to see the post-mortem report treated as a priority – not only does it potentially have an impact on a future pregnancy but also it has a huge impact on families whose lives are kept on emotional hold while they await results.
Recommendation 9
In the absence of the large charities and interested industry that fund the bulk of research for other health conditions, we recommend that the Welsh Government, through the National Institute for Social Care and Health Research’s Clinical Research Centre, commission a comprehensive piece of work on the underlying causes of stillbirth. This work should be undertaken in cooperation with health professionals and academics with expertise in this field, and should draw on international knowledge of stillbirth. This work should be completed by the end of this Assembly.
The Welsh Government progress report points to the collaboration with the Scottish-led AFFIRM study (which Sands part funds along with Scottish Government and Tommy’s). The study is trialling a package of care for women who report changes in their baby’s movements, to determine if it impacts on stillbirth rates. The care package, which includes information for women as well as protocols for care and training for health care professionals, is based on NICE antenatal guidance and RCOG Green Top guidance.
Hospitals from across the UK are participating, including two Welsh Health Boards: Aneurin Bevan and Betsi Cadwaladr - totalling five Welsh hospitals. Hospitals are randomised into clusters which then join the study at regular intervals. The study began roll out in mid 2014 and will continue into 2016. We hope the study will contribute new evidence to inform improved guidelines, care and patient information.
While the AFFIRM study looks at one aspect of stillbirth reduction, the HSCCs recommendation was to commission “a comprehensive piece of work on the underlying causes of stillbirth.” Clearly the AFFIRM study only partially fulfils this recommendation, and we would welcome commitment to further stillbirth research, including funding.
Sands sponsors the Stillbirth Clinical Study Group within the RCOG (Royal College of Obstetrics and Gynaecology), which identifies gaps in research and supports development of new research studies. Wales is represented on this group; the group’s expertise can be used to advise on research priorities. More research funding is essential to support work to understand better the causes of stillbirth and develop new effective interventions to prevent more deaths.
